Fact Checked
Intus Healthcare’s writers, customer service team, and sleep experts review and ensure this information is accurate.
Last updated on March 28th, 2025 at 01:41 pm
Sleep Apnoea is a common disorder that affects millions of people worldwide. It is often characterised by interrupted breathing during sleep, resulting in poor sleep quality and excessive daytime fatigue.
While the physical health implications of Sleep Apnoea are widely known, the impact on mental health is often overlooked. However, recent research is shedding more light on this link and indicating sleep deprivation could contribute to mental health disorders(1).
If this is the case, diagnosing and treating sleep disorders such as Sleep Apnoea could help alleviate these mental health issues.
Table of Contents
Understanding the Link: Sleep and Mental Health
Various research has extensively studied and confirmed the link between sleep and mental health.
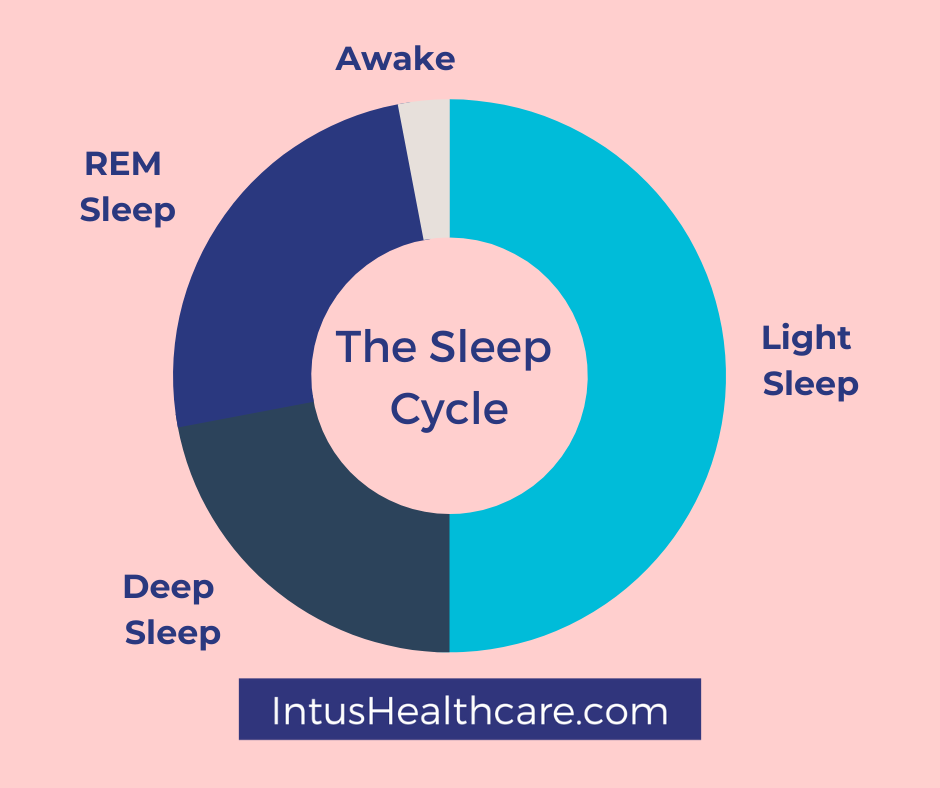
When we sleep, we experience different sleep cycles, but there are technically two categories: non-rapid eye movement (NREM) and rapid eye movement (REM).
Together, these two types of sleep make up a single cycle in which your brain progresses sequentially through each stage of sleep: wake, light sleep, deep sleep, and REM.
The stages of sleep play a significant role in our emotional and mental well-being.
The first two stages involve relatively light sleep, building to a deeper state of rest and then REM. In the third stage, the body repairs muscle and tissue damage from the day and boosts the immune system.
Deprivation of REM sleep, which occurs approximately 90 minutes after falling asleep, has been shown to increase the risk of mental health problems(2). During REM sleep, the brain is more active and helps consolidate information from the previous day, contributing to emotional health.
Sleep Apnoea and Mental Health
Obstructive Sleep Apnoea (OSA), the most common type of Sleep Apnoea, leads to sleep deprivation due to frequent interruptions in breathing. It is characterised by narrowing the upper airways during sleep, resulting in breathing pauses and frequent awakenings.
Sleep deprivation, whether caused by Sleep Apnoea or other sleep disorders, has been associated with an increased risk of depression and anxiety. In fact, it is estimated that 75% of depressed patients have insomnia symptoms, and hypersomnia (excessive tiredness) is present in about 40% of young depressed adults(3).
The constant interruptions in breathing throughout the night create a sense of fear and restlessness, leading to increased anxiety levels. Symptoms such as heavy snoring, choking or gasping during sleep, and severe daytime tiredness are common indicators of Sleep Apnoea. These symptoms, combined with the lack of quality sleep, contribute to heightened anxiety levels.
Individuals with a history of insomnia or sleep disorders are three times more likely to experience depression(4). Moreover, sleep disorder sufferers are less likely to respond to treatment for depression, highlighting the importance of addressing sleep issues alongside mental health conditions.
The constant disruption to sleep with any sleep disorder can have a significant impact on mood and emotional vulnerability.
Mental health conditions can often co-occur and have an impact on one another as well as on a person’s sleep. For instance, it’s common for individuals to experience both depression and anxiety, and studies have found that people who have both of these conditions tend to have worse sleep quality compared to those who have only depression or anxiety(5). Other factors related to mental health, such as perception of pain, can also affect sleeping patterns. Therefore, it’s important to address all aspects of mental well-being when managing sleep problems.
To effectively manage mental health problems related to sleep, it is crucial to address and treat the underlying sleep disorder. Undertaking a sleep test is the first step towards diagnosis and starting the appropriate treatment. By improving sleep quality, individuals with Sleep Apnoea can experience a reduction in anxiety levels and overall stress.
Taking Steps Towards Better Mental Health
Diagnosing and treating sleep disorders, including Sleep Apnoea, is crucial in managing mental health conditions. Individuals are often unaware of their Sleep Apnoea causing continuous interruptions throughout the night. A sleep study can determine the presence and severity of Sleep Apnoea and guide you to the appropriate treatment plan.
Continuous positive airway pressure therapy (CPAP) is the most effective treatment for moderate to severe OSA. It involves wearing a mask that delivers pressurized air, preventing narrowing the upper airways.
Alongside medical interventions, implementing lifestyle changes can also improve sleep quality.
This could include:
- Quitting Smoking
- Avoiding alcohol before bedtime
- Establishing a regular sleep routine
- Creating a relaxing bedtime routine
- Practicing good sleep hygiene
- Seeking professional help.
By taking these steps, you can improve your sleep quality and reduce mental health symptoms, leading to a better quality of life.
If you suspect that you may have sleep problems or exhibit symptoms of Sleep Apnoea, it is crucial to consult with a healthcare professional and undergo a sleep study. Early diagnosis and appropriate treatment can lead to better sleep and improved mental health.

Home Sleep Apnoea Test
The test monitors your heart rate, snoring intensity, blood oxygen levels, body positioning, and more, providing accuracy comparable to testing used in sleep clinics for in-depth sleep analysis.
The simple-to-use test takes just one night to complete, and results are returned within two working days after completion.
Our experienced NHS-qualified sleep professionals independently analyse all studies, providing follow-up advice and support.
About Our Editorial Team
Danni is a degree-educated content writer passionate about helping those with Sleep Apnoea sleep better; she works closely with our clinical and customer care teams to ensure that each article is thoroughly researched and accurate.
Her writing aims to inform, support, and advise readers about Sleep Apnoea, helping to raise awareness and promote effective treatment options.
She has written many health-focused articles, reaching hundreds of readers annually, to help people sleep better and live healthier lives.
Lateisha King is an experienced Sleep Clinician with advanced training in polysomnography and respiratory health.
With over six years of experience, including at the prestigious Guy’s and St Thomas’ NHS Foundation Trust Hospital, she has conducted and reviewed more than 500 diagnostic sleep studies.
Her expertise in sleep science ensures that all articles align with the latest data and treatment protocols, providing readers with trustworthy and practical advice to improve their sleep health and overall well-being.
REFERENCES
- Scott, A. J., Webb, T. L., Martyn-St James, M., Rowse, G., & Weich, S. (2021). Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Medicine Reviews, 60, 101556. Available at: https://doi.org/10.1016/j.smrv.2021.101556 . Accessed: 19.09.23
- Anderson, K., & Bradley. (2013). Sleep disturbance in mental health problems and neurodegenerative disease. Nature and Science of Sleep, 61. Available at: https://doi.org/10.2147/nss.s34842. Accessed: 19.09.23
- Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in Clinical Neuroscience, 10(3), 329–336. Available at: https://doi.org/10.31887/dcns.2008.10.3/dnutt. Accessed: 19.09.23
- Ford, D. E. (1989). Epidemiologic study of sleep disturbances and psychiatric disorders. JAMA, 262(11), 1479. Available at: https://doi.org/10.1001/jama.1989.03430110069030. Accessed: 19.09.23
- Oh, C.-M., Kim, H. Y., Na, H. K., Cho, K. H., & Chu, M. K. (2019). The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: A population-based study. Frontiers in Neurology, 10. Available at: https://doi.org/10.3389/fneur.2019.00849. Accessed: 19.09.23





