Fact Checked
Intus Healthcare’s writers, customer service team, and sleep experts review and ensure this information is accurate.
Last updated on October 14th, 2024 at 02:14 pm
Nasal congestion can worsen Sleep Apnoea due to its impact on airflow through the upper airway.
This article will explain how the common cold can affect your Sleep Apnoea and ways to solve it.
Table of Contents
Nasal congestion and Sleep Apnoea
Nasal congestion is commonly characterised by a blocked, stuffy or runny nose and can be uncomfortable at the best of times. It can make it particularly difficult to get a good night’s sleep, exasperating symptoms of Sleep Apnoea.
People who experience consistent chronic nasal congestion can double their risk of the sleep disorder Obstructive Sleep Apnoea (OSA). Mainly due to allergic rhinitis, making sufferers 1.8 times more likely to develop moderate to severe OSA compared to those without nasal congestion. The nasal obstruction increases airway resistance and encourages mouth breathing, which leads to more airway collapses during sleep, worsening OSA symptoms (1).
Can Nasal Congestion Cause Sleep Apnoea?
Yes, nasal congestion, rhinitis and sinusitis have been found to cause Sleep Apnoea.
How does nasal congestion cause OSA?
Sinus congestion increases breathing resistance, snoring, apnoea events, hypopnoea events and mouth breathing. If the sinus inflammation is left untreated for a long period, it can contribute to developing Sleep Apnoea as it prevents the body from maintaining a steady airflow.
Additionally, increasing or switching to mouth breathing makes it harder and less effective to maintain an open airway than nasal breathing, increasing apnoeas. When the nose is congested, the body has to generate more negative pressure to pull air in through the narrowed nasal passages. This increased pressure can cause the throat tissues to collapse, worsening OSA.
Congestion worsens the physical symptoms and disrupts sleep quality. It can cause more awakenings during the night, making the person more aware of the discomfort and decreasing the overall effectiveness of OSA treatments.
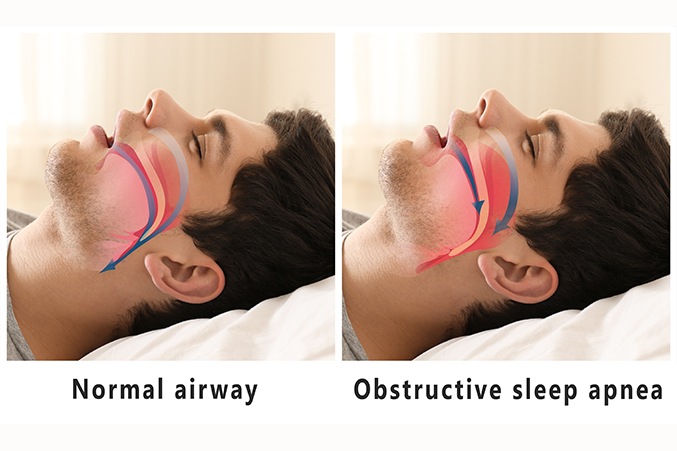
Normal airway vs OSA
Non-allergic Rhinitis and Sleep Apnoea
Although chronic nasal congestion can result from allergic rhinitis, such as pollen associated with hay fever, people can also suffer from non-allergic rhinitis.
An allergen does not cause inflammation in the nose. Inflammation is often due to swollen blood vessels and a build-up of fluids. When you have a cold or a viral infection, the nasal passages can swell, stimulating the mucus glands.
However, due to the illness, they cannot clean themselves effectively. This can lead to a blocked or runny nose, sneezing, and reduced sense of smell, which are symptoms of nasal congestion.
Non-allergic rhinitis can display symptoms similar to rhinitis caused by allergens. Aside from viral infections and colds, further causes could be medications, nasal decongestants, hormonal imbalance, nasal tissue damage and environmental factors such as smoke, weather changes, paint fumes and stress.
The mucus which builds up due to non-allergic rhinitis contains bacteria that cause inflammation. These inflamed nasal passages resulting from non-allergic rhinitis can lead to an infection called acute sinusitis.
However, if this is left untreated, it can develop into chronic sinusitis with chronic nasal congestion. And this consequence can take much longer to clear.
As well as colds, sinusitis can result from environmental factors such as swimming in polluted water. Smoking can also make you more susceptible to this condition.
Nasal congestion could also result from structural issues in the nose, such as the physical disorder septal deviation, which results in largely constant nasal congestion.
Whereas other forms of non-allergic rhinitis can be treated with antibiotics, nasal sprays or possibly steroids, a structural abnormality with the nose may require surgery.
Remedies for Nasal Congestion
Nasal congestion can double the risk of OSA by completely blocking the airways. You should consult your doctor if you are constantly experiencing congestion. Solutions can be made at home or bought from a pharmacy to relieve congestion.
If there are environmental triggers which accelerate your congestion, such as smoke, these should be avoided.
SinuPulse Nasal Irrigation
Nasal irrigation is a proven technique that has been used for centuries, such as the SinuPulse Elite.
No more netipots or ineffective nasal sprays. Instead, the SinuPulse Elite offers a convenient and comprehensive solution to sinus problems. The pulsating mechanism makes nasal irrigation faster, more comfortable and more effective than ever before.
Choose between a soothing mist or cleansing jet spray. Both are included with the device.
The SinuPulse Elite Advanced Nasal Sinus Irrigation System was engineered by a team of Swiss professionals with over 30 years of sinus irrigation experience. It delivers a natural, soothing, drug-free saline solution – via a gentle water flow or mist at a pressure you control to help relieve unpleasant symptoms. This is because the specially formulated salts help draw out blockages and heal delicate nasal tissue.
Switch to a Full Face Mask
If you suffer from congestion and are using a nasal mask, consider switching to a full face style. This benefits your therapy by ensuring you receive the airflow from your CPAP machine.
A nasal mask used when your nose is blocked prevents your airways from staying open as your body can not intake the airflow.
Use a humidifier
If you use a CPAP machine, adding a humidifier warms the airflow, so you are not breathing in cold air, which can worsen your symptoms. Most machines have a humidifier option that can be added to your therapy.
The Risk Factors of Obstructive Sleep Apnoea
Obstructive Sleep Apnoea (OSA) involves airways that become blocked or partially blocked as you sleep, causing continuous breathing pauses. Commonly those with OSA wake up gasping for air and aren’t always aware of the continuous waking up. Sleep Apnoea is usually detected by a partner noticing choking during sleep and breathing pauses.
Related post: Signs your partner has Sleep Apnoea
One of the main symptoms of OSA is constant fatigue due to frequent interruptions in sleep. Other symptoms include heavy snoring, concentration and motivation difficulties, morning headaches, waking up with a dry or sore throat, anxiety and depression.
It can be too easy to put symptoms like fatigue down to the stresses and strains of modern-day life. When left untreated, OSA can lead to serious health problems, including:
- Heart disease
- Type 2 diabetes
- High blood pressure
- Liver damage
- Pregnancy complications
- Increased risk of injury from accidents due to fatigue (10-20% of driving crashes are due to driving fatigue)
The Importance of Testing for Sleep Apnoea
Diagnosis is key to receiving the appropriate treatment for your level of Obstructive Sleep Apnoea. A simple in-home sleep test can be completed for one night in the comfort of your own home.
With this test, you will be sent a small finger probe and chest sensor. The test will record blood oxygen levels and heart rate while you sleep.
Once completed, your data will be analysed by a sleep expert.
Testing is a critical first stage in addressing the symptoms of Obstructive Sleep Apnoea.

What is a Sleep Test?
The sleep test determines if you have Sleep Apnoea. It monitors your heart rate, snoring intensity, blood oxygen levels, body positioning, and more, providing accuracy comparable to testing used in sleep clinics for in-depth sleep analysis.
The simple-to-use test takes just one night to complete, and results are returned within two working days after completion.
Our experienced NHS-qualified sleep professionals independently analyse all studies, providing follow-up advice and support.
OSA Treatment
Treating nasal congestion helps keep the airways open and reduces the risk factor for OSA.
However, if your In-Home Sleep Test results have led to a sleep disorder diagnosis, you will be recommended appropriate treatment options for the level of OSA you have.
For mild to moderate levels of OSA, lifestyle changes may be enough to reduce the symptoms, such as:
- Losing weight
- Exercising
- A healthier diet
- Quitting smoking
- Reducing alcohol consumption
- Reducing stress
Positional Therapy
An option is to wear a Positional Sleep Therapy device. These devices prevent you from sleeping on your back to help relieve breathing pauses.
Mouth Guard or an Oral Appliance
You may also be advised to wear a mouthguard-style device as you sleep, which pushes the lower jaw down to keep the airways open and aid breathing. These oral appliances are known as Mandibular Advancement Devices.
CPAP Therapy
For more severe OSA levels, the leading treatment is Continuous Positive Airway Pressure (CPAP) therapy which uses a machine to supply a steady stream of pressurised air through a mask while you sleep, helping maintain open airways and prevent chronic snoring.
Bringing it all together
As nasal congestion robs your body of the restorative sleep that’s necessary for good health, it’s best to discuss your problem with your doctor.
You might also take an In-Home Sleep Apnoea test to learn if you have Obstructive Sleep Apnoea. It’s the first step toward a healthier, longer, more satisfying life.
Alternatively, take our free online OSA risk assessment.
For any help and advice, contact us.
References:
- M. Kohler, K. E. Bloch, J. R. Stradling. 2007. European Respiratory Journal. The role of the nose in the pathogenesis of obstructive sleep apnoea and snoring. Available at: https://erj.ersjournals.com/content/30/6/1208. Accessed: 14.10.2024.